Better Laid Plans of Mice and Men
Adapted from a line in “Ode to a Mouse” from fellow countryman Robert Burns, the phrase, “the best-laid plans of mice and men often go awry”, indicate that no matter how carefully a project is planned, something may still go wrong with it unfortunately speaks to the reality of clinical trials for novel therapeutics, with approximately only 11% of drugs that begin phase I clinical trials eventually being licensed. Today, mouse models remain among the most valuable tools in cancer research, especially in the pre-clinical phases of drug discovery. Researchers use them for many types of studies – from gaining insights about cancer biology pathways to identifying new treatments and their mechanisms of action. The term ‘humanized’ mouse, however, describes a model in which various types of human genes, cells, and/or tissues are introduced into the mouse to function as they would in humans. For this purpose, several types of immunodeficient mice, which do not reject xenografts and support the differentiation and growth of xenotransplanted cells and tissues, have become indispensable in cancer research and have improved success of novel cancer therapeutics.
March 30, 2022
Research in the field of humanized mice began in the late 1980s, a few years after the discovery of mice with severe combined immunodeficiency (SCID) resulting from a spontaneous mutation, specifically, Prkdcscid, (protein kinase, DNA activated, catalytic polypeptide; severe combined immunodeficiency allele) identified in a colony of C.B-17 mice. This functional inactivation then led to defective DNA repair and repair-dependent somatic V(D)J recombination of B and T cell receptor-encoding genes, resulting in the absence of mature B and T lymphocytes. Taking advantage of the severe immunodeficiency of these animals, several groups then successfully transplanted human PBMCs (peripheral blood mononuclear cells), human bone marrow cells, human fetal tissues, or human HSPCs (hematopoietic stem cells) into SCID or equivalent recipient mice models. These humanized mice can accept the xenografted elements of the human immune system and as a result, the have an immune system that is part mouse part human. Next, by xenografting cancer cell lines or patient tumor explants into such mice, the effect of an intervention such as a drug treatment on the xenograft in the context of an intact immune system can be investigated. Thus, establishment of cell-line-derived xenograft (CDX) and patient-derived xenograft (PDX) into humanized mouse models has been a remarkable stride for facilitating diverse applications in the exploration of cancer pathogenesis, and the evaluation of therapeutic effects.
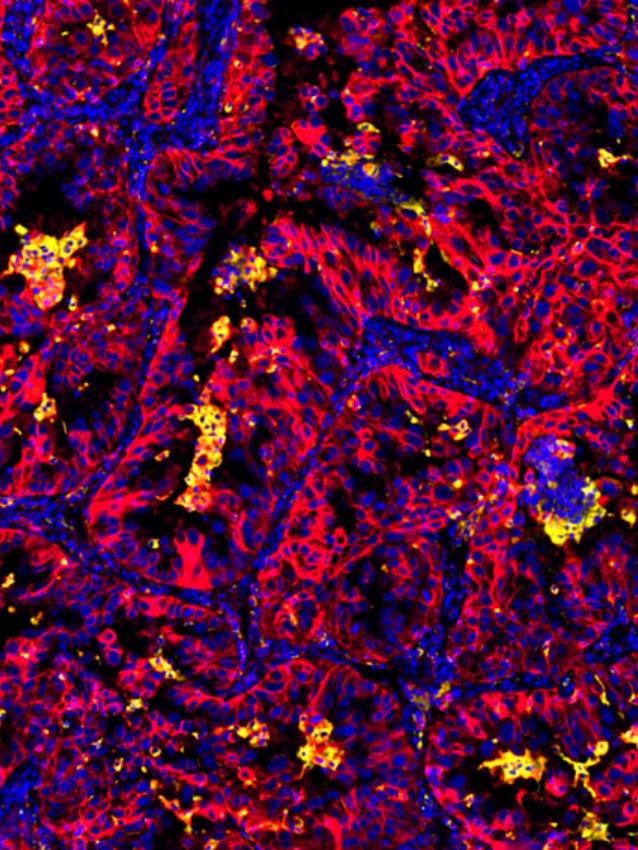
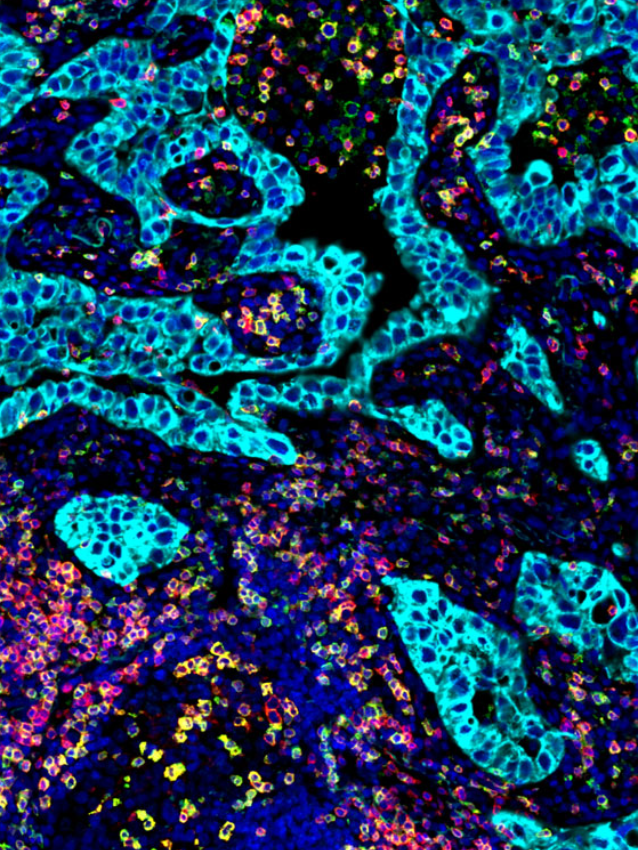
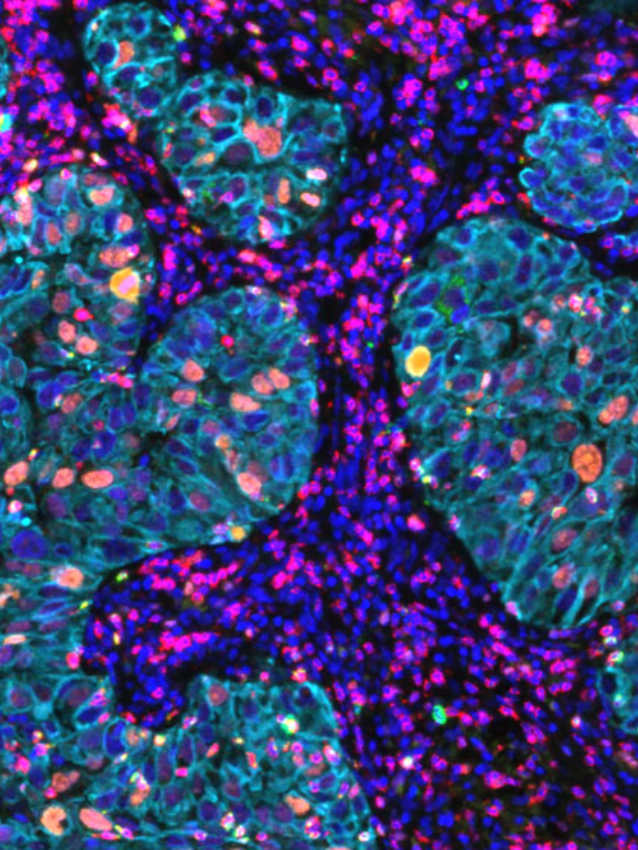
While CDX models are less time-consuming to generate, the in vitro culture step before engraftment typically leads to substantial loss of primary tumor features. PDX mice on the other hand, largely retain the key characteristics of the patient’s tumors, including histological features, genomic signatures, and the heterogeneity of cells in a tumor mass, particularly the tumor immune microenvironment (TiME), visualized using multiplexed immunofluorescence (mIF) techniques. Therefore, these mouse models can potentially serve as a more accurate platform for predicting therapeutic outcomes.
An area of active research is resistance mechanisms to immune checkpoint blockade therapy, and to identify therapeutic combination strategies to enhance effectiveness for treatment in these tumor types. For example, a recent publication (2) explored why most hepatocellular carcinoma (HCC) patients currently respond poorly to anti-PD1 therapy.
Hepatocellular carcinoma (HCC) remains one of the most prevalent and life-threatening malignancies globally. Unfortunately, over 60% of HCC patients are diagnosed at advanced stages, and therefore cannot undergo curative surgery. While ICB (immune checkpoint blockade) therapies, especially with antibodies against the PD1/PD-L1 signaling axis, have made impressive breakthroughs in cancer treatment, clinical trials of HCC patients have not shown statistically significant improvements owing to primary or acquired anti-PD1 resistance. The group noted that the zinc finger protein, ZFP64 was frequently upregulated in HCC tissues of anti-PD1 resistant patients, with additional experiments indicating that a PKCα/ZFP64/CSF1 axis was critical for triggering immune evasion and anti-PD1 tolerance. Of interest, Gö6976, an inhibitor of PKCα, when introduced to both PDX and orthotopic xenograft tumor models, significantly suppressed tumor progression and altered the TiME via the PKCα/ZFP64/CSF1 axis in HCC, as measured using mIF techniques. Importantly, the group presented extensive evidence that the combined treatment of Gö6976 with anti-PD1 could synergistically improve the survival of tumor-bearing PDX mice, especially in the subset overexpressing ZFP64.
With the accumulating evidence from many publications (3,4), the use today of PDX and “better” improved humanized mouse model designs, as well as updated methods to visualize cell and spatial contexture, have become highly effective in predicting the efficacy of both conventional and novel anti-cancer therapeutics. Indeed, ongoing areas of research now afford “co-clinical trials,” in which pre-clinical investigations in vivo and clinical trials can be performed in parallel or sequentially to assess drug efficacy in mice (PDX) and men (patients).
Historically, detection of protein targets from different species in the same tissue section was difficult due to dependence on species-specific secondary antibodies (e.g. goat anti mouse secondary antibody to detect an mouse antibody made against a human protein). Ultivue’s direct antibody labeling technology eliminates detection barriers due to species, allowing rapid creation of multiplex reagents against targets from multiple species in the same multiplex panel. For more information on how to incorporate multiplexed immunofluorescence from your PDX or humanized mouse model and derive valuable spatial information from the tumor microenvironment, please visit www.ultivue.com.